Consider the following scenario, of which the details have been changed to protect the individual’s identity: Staff Sergeant Ford is a 30-year-old Marine who grew up in the Rocky Mountain West. SSgt. Ford grew up around guns—his parents were both competitive shooters and he spent many hours at firearm ranges. His parents were responsible firearm owners and instilled in SSgt. Ford from an early age the importance of secure firearm storage. They kept all their firearms—rifles and pistols alike—unloaded and stored in a gun safe to which only the adults had keyed access. Shortly after SSgt. Ford graduated from high school, he joined the Marines and subsequently experienced two combat deployments to Afghanistan. After acquiring personal firearms, SSgt. Ford, too, kept his firearms unloaded and in a gun safe. While in Afghanistan, SSgt. Ford and his unit sustained multiple instances of small arms fire and improvised explosive device (IED) attacks. Fortunately, SSgt. Ford was never physically injured during these attacks; nevertheless, he witnessed the deaths of multiple fellow Marines as well as civilians. Upon return home to the United States, SSgt. Ford had difficulty shaking the memories of these traumatic deaths. He experienced regular nightmares and was easily startled by loud noises, such as a car door slamming. Although he never told anyone, his journal entries suggested he experienced marked guilt for the deaths of fellow Marines, writing, in part, “It should’ve been me. Why didn’t I stop the IED?” These and other thoughts kept him up at night, and although he never masked the struggles with alcohol or other substances, he would push the terrifying thoughts away as much as possible—often to no avail. SSgt. Ford also grew increasingly concerned about his safety while in the US, although there were no clear environmental reasons suggesting he was actually unsafe. In response to these concerns, though, he would scan buildings in which he entered, and he remained “on guard” for potential dangers. As part of this hypervigilance to a potential threat, SSgt. Ford began carrying a loaded pistol wherever he went—a marked shift from pre-deployment in the secureness of his firearm storage practices. Five months following his return to the US, SSgt. Ford tragically killed himself via a self-inflicted gunshot wound. Although SSgt. Ford never accessed mental health care services, a postmortem suicide death review revealed that SSgt. Ford likely would have been diagnosed with post-traumatic stress disorder (PTSD).1
There are several features related to this brief case narrative worth highlighting:
- Veterans are more likely than nonveterans to use a firearm to enact their suicide (approximately 70 percent vs. 50 percent), and this risk is elevated even more so shortly after leaving the military;
- The nonsecure storage of firearms is associated with an elevated risk for suicide;
- Veterans are at increased risk relative to nonveterans to develop PTSD; and
- PTSD is associated with elevated risk for both suicide and nonsecure firearm storage practices.
The increased risks among veterans, relative to the general population, of suicide (including firearm suicide) and PTSD are well-documented. Less has been discussed, however, regarding the intersection between PTSD symptoms and firearm storage practices. If individuals with PTSD are more likely to store their firearms in a nonsecure manner (e.g., loaded, unlocked), and if both PTSD and nonsecure firearm storage are risk factors for suicide, then greater attention is needed to promote secure firearm storage practices among individuals with PTSD.
Why might PTSD impact firearm storage practices? PTSD, according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), is characterized in part as the development of characteristic symptoms following exposure to a life-threatening or traumatic event. These characteristic symptoms include intrusive reminders, avoidance, changes in thinking patterns and mood, and changes in physiological reactivity (e.g., hypervigilance to threat). PTSD may be diagnosable when a certain combination of PTSD symptoms arise, persist for at least one month, and cause clinically significant distress or impairment.
A cardinal feature of PTSD is a hypervigilance to threat, which can manifest in both beliefs (e.g., “The world is entirely dangerous”) and behaviors. One of the behaviors that has been observed in association with PTSD is engaging in nonsecure firearm storage practices. As we saw in SSgt. Ford’s vignette, following the development of PTSD symptoms, he shifted from secure to nonsecure firearm storage practices, in part by carrying his firearm to be “at the ready” for potential threats in the environment.
Greater PTSD symptoms were associated with elevated odds of reporting nonsecure firearm storage practices, defined as storing a firearm loaded and/or in a nonsecure location. Interestingly, when examining the specific facets of PTSD, the hyperarousal symptoms—defined in part by a behavioral repertoire that manifests due to threat-related concerns—were uniquely associated with nonsecure firearm storage practices.
Multiple studies and a recent systematic review have found that individuals with PTSD (or elevated PTSD symptoms) are more likely than individuals without PTSD to store their firearms in such a nonsecure manner. In one study, my colleague Dr. Michael Anestis (New Jersey Gun Violence Research Center) and I examined this question with respect to 327 members of the Mississippi National Guard, all of whom reported personal firearm ownership. We assessed PTSD symptoms via a commonly used and well-validated self-report measure, the PTSD Checklist for DSM-5 (PCL-5). Greater PTSD symptoms were associated with elevated odds of reporting nonsecure firearm storage practices, defined as storing a firearm loaded and/or in a nonsecure location. Interestingly, when examining the specific facets of PTSD, the hyperarousal symptoms—defined in part by a behavioral repertoire that manifests due to threat-related concerns—were uniquely associated with nonsecure firearm storage practices. This suggests that, among a military population, PTSD-related fear might prompt firearm behaviors that increase one’s risk for suicide.
What can be done to address nonsecure firearm storage practices among individuals with PTSD? Efforts to promote secure firearm storage are recommended by healthcare organizations, the US Department of Defense, and the US Department of Veterans Affairs (VA). There are multiple ways to promote secure firearm storage. One commonly recommended approach is lethal means safety counseling (LMSC), which refers to guided discussions to help an individual identify personalized firearm storage practices. LMSC has been shown to prompt secure firearm storage in military populations. LMSC commonly occurs in the context of clinical encounters, either in medical (e.g., primary care, emergency department) or psychiatric (e.g., outpatient, inpatient) settings. Critically, however, research has shown that individuals who die by firearm suicide are less likely than individuals who die by other means to have accessed mental healthcare services before their death. Thus, it is important to consider nonclinical, public health approaches to reducing the risk of firearm suicide (and other firearm-involved injuries).
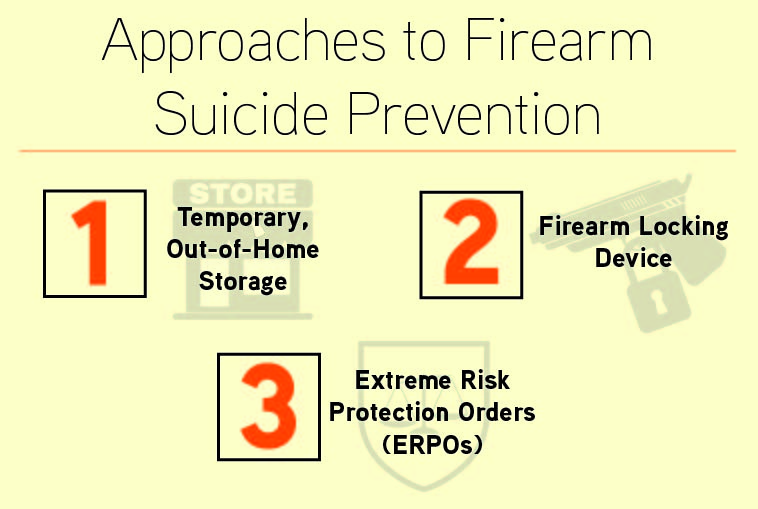
These public health approaches include the temporary, out-of-home storage of personal firearms, including at firearm retailers and gun shops; while this method can promote distance between oneself and one’s firearm during at-risk periods, there are nuanced differences between states in the legality of temporary firearm transfers and important questions remain unanswered regarding retailer/shop liability and conditions under which a firearm may be returned to its owner. Another approach involves the distribution of firearm-locking devices or offering financial incentives (e.g., coupons) to encourage firearm-locking device acquisition and use. Finally, an additional public health approach involves extreme risk protection orders (ERPOs), which are civil restraining orders that temporarily prohibit at-risk individuals from either possessing or purchasing a firearm, are a novel approach allowed in some jurisdictions and preliminary evidence suggests ERPOs are associated with a reduced risk of firearm suicide. While these clinical and public health approaches are not necessarily specific to PTSD, there are efforts currently underway to adapt existing approaches to have a trauma-informed lens. This is particularly important considering recent work conducted by my colleagues and I showing diminished efficacy of existing LMSC practices for military personnel with elevated PTSD symptoms.
Thankfully, most veterans, even combat-exposed veterans, neither develop PTSD nor think about, attempt, or die by suicide. Yet, we know that veterans are particularly affected compared with the general population. As clinicians, policymakers, and community members, we owe it to our veterans, including those with experiences similar to SSgt. Ford, to examine all possibilities for suicide prevention. This includes a consideration of the intersection between PTSD—consequences not of just war but also military service and civilian experiences—and firearm storage practices. A critical first step is ensuring sufficient resources exist to screen for and treat PTSD symptoms and cooccurring mental health conditions among veterans. Importantly, not all veterans are eligible for care within the VA, and a sizable proportion of veterans elect to receive care from non-VA community partners. Mental health care services, therefore, must be readily available regardless of a VA connection. Because the causes of suicide are multifactorial, suicide prevention programming among veterans must also attend to nonclinical contributors, including social disconnectedness, financial difficulties, and, broadly, access to lethal means such as firearms. By investing in veteran suicide prevention, veterans like SSgt. Ford will have a better chance of surviving and thriving.
ABOUT THE AUTHOR
Ian H. Stanley is an assistant research professor at the Department of Emergency and Medicine, the psychological health lead at the CU Center for COMBAT Research and the military and veteran lead at the CU Firearm Injury Prevention Initiative at the University of Colorado, and an affiliate scholar of the Regional Gun Violence Research Consortium
[1] The identity and details of the case narrative have been edited to protect the individual’s privacy.

